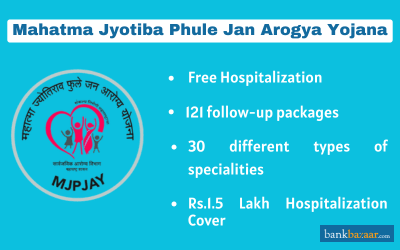
Mahatma Jyotiba Phule Jan Arogya Yojana
The Rajiv Gandhi Jeevandayee Arogya Yojana, renamed Mahatma Jyotiba Phule Jan Arogya Yojana, is a scheme that is backed by the State Government of Maharashtra. The scheme offers health insurance benefits to people belonging to BPL and APL households.
Rajiv Gandhi Jeevandayee Arogya Yojana (RGJAY), presently known as Mahatma Jyotiba Phule Jan Arogya Yojana is a health insurance scheme introduced by the Maharashtra state government. The scheme was launched to provide free hospitalization and medical care to the Below Poverty Line (BPL) and Above Poverty Line (APL) families.
RGJAY provides free medical facilities on 30 different types of specialities, 121 follow-up packages, and 971 procedures. Apart from this, a beneficiary family will receive Rs.1.5 lakh hospitalization cover if any of the family members undergo medical treatment in a hospital which is listed under this scheme.
What is Covered?
Under the RGJAY scheme, APL and BPL families can avail of free hospitalization for the following specialities:
- General surgery
- Opthalmology surgery
- ENT surgery
- Cardiac and cardiothoracic surgery
- Paediatric surgery
- Gynaecology and obstetrics surgery
- Plastic surgery
- Nephrology
- Burns
- Endocrinology
- Pneumonia
- Diarrhoea
- Hernia
- Appendicitis
- Snakebite (Ventilation support for snakebite)
How to Register for RGJAY Scheme?
Given below are the steps to register for the RGJAY scheme:
Step 1 - Visit your nearest empanelled hospital and provide your valid ration card and a photo ID to the Medical Coordinator.
Step 2 - The Medical Coordinator will capture certain information like admission notes and test reports on the database.
Step 3 - The pre-authorization request will be forwarded to the insurance company that is associated with the RGJAY scheme.
Step 4 - The request will also be reviewed by the medical specialists, doctors and the insurer.
Step 5 - Once the documents are reviewed, the claim will be verified by the insurer.
Step 6 - The beneficiary will receive cashless medical treatment and hospitalization services.
Step 7 - The beneficiary can also avail of free follow consultation and diagnostics services up to ten days from the date of discharge.
How to Login to RGJAY Scheme?
Given below are the steps to log in to RGJAY scheme:
Step 1 - Visit the Official Website at https://www.jeevandayee.gov.in
Step 2 - Enter your ‘Username’ and ‘Password’.
Step 3 - Click on the ‘Login’ button to enter the portal.
Eligibility Criteria:
Here are the eligibility criteria to register for RGJAY Scheme:
- Families having Yellow Ration Card, Annapurna Card, Orange Ration Card, and Antyodaya Anna Yojana (AAY) are eligible to register for the RGJAY scheme.
- Farmers belonging to 14 agriculturally distressed districts of Maharashtra having white ration cards are also eligible.
Documents Needed for Rajiv Gandhi Jeevandayee Arogya Yojana:
Given below are the documents which are needed to be submitted to avail of RGJAY scheme facilities:
- White, orange, or yellow ration card
- Voter ID card
- Aadhar card
- PAN card
- Driving license
- School ID card
RGJAY Claim Settlement Process:
Given below is the step-by-step claim settlement process for the RGJAY scheme:
Step 1 - Visit your nearest empanelled hospital and get a diagnosis for your medical condition.
Step 2 -The hospital will send a request to the insurance provider for pre-authorization.
Step 3 - Once the pre-authorization is received, the treatment for the diagnosed medical condition will start.
Step 4 - Once the medical treatment gets over, the empanelled hospital will provide all the important documents to the insurance provider
Step 5 - The insurance provider will go through the documents and approve the claim.
RGJAY Toll Free Number:
You can get in touch with their toll-free number 1800 233 2200.
FAQs on Mahatma Jyotiba Phule Jan Arogya Yojana
- What is Mahatma Jyotiba Phule Jan Arogya Yojana health card?
Mahatma Jyotiba Phule Jan Arogya Yojana health card is issued as an ID of the beneficiary families under the scheme.
- Is RGJAY a cashless health insurance scheme?
Yes. RGJAY is a cashless health insurance scheme.

Disclaimer
Credit Card:
Credit Score:
Personal Loan:
Home Loan:
Fixed Deposit:
Copyright © 2026 BankBazaar.com.
