Bhamashah Swasthya Bima Yojana
The Bhamashah Swasthya Bima Yojana is a scheme that is open to residents of Rajasthan. The scheme aims to offer cashless services to IPD patients. Families that are covered under the NFSA and RSBY can register for this scheme.
Bhamashah Swasthya Bima Yojana, also known as BSBY is a cashless health insurance scheme introduced by the Rajasthan Government on 13 December 2015. Families which are eligible for this scheme can avail free medical treatment of up to Rs.30,000 for general illness and Rs.3 lakhs for the critical illness.
People who are covered under Rashtriya Swasthya Bima Yojana (RSBY) and National Food Security Act (NFSA) are eligible for BSBY. Rajasthan Government has collaborated with New India Assurance Company to provide cashless health insurance to poor and needy people. The insurance company has the most attractive insurance plans that can be availed by paying affordable premiums.
What is Covered Under this Scheme?
Given below are the list of expenses which are covered under Bhamashah Swasthya Bima Yojana:
- BSBY provides cashless hospitalization facility which covers the complete expenses incurred by the insured.
- The insured can avail the cashless hospitalization facility in any government and private network hospitals.
- The scheme general provides illness coverage of up to Rs.30,000 and Rs.3 lakh for critical illnesses.
- BSBY also covers pre hospitalization expenses for maximum seven days before getting admitted into the hospital.
- The insured will also get post-hospitalization coverage for up to 15 days after he or she gets discharged from the hospital.
- Transportation allowance up to Rs.500 is provided for cardiac and polytrauma cases.
- In addition, the insured can receive cashless treatment for OPD (Outpatient Department) cases.
Apart from this, the insured can choose their desired package from 1,045 packages under general illnesses, 170 packages for government hospitals, and 500 packages under critical illnesses. The scheme covers expenses related to medicines, doctor consultation fees, bed charges, nursing charges, blood, implants, boarding fees, food expenses, and transportation allowance while hospitalized.
How to Apply Under Bhamashah Swasthya Bima Yojana?
As the scheme is designed only for the people who are below poverty line, the application procedure is done on an offline basis. Given below are the steps which are to be followed while applying under Bhamashah Swasthya Bima Yojana:
Bhamashah Swasthya Bima Yojana Online Application:
- The interested people should visit any of the network hospitals.
- They have to get in touch with the BSBY official in the network hospital.
- The applicant should submit all the necessary documents.
- The BSBY official will fill up the application form on behalf of the individual.
Who is Eligible?
The following are the eligibility criteria for Bhamashah Card:
- The individual should be the resident of Rajasthan.
- The cardholder should belong to a BPL family.
- The applicant should have her bank account opened under Bhamashah Scheme.
Documents Required:
Given below is the list of documents which are required to be submitted to file a claim under BSBY:
- Patient’s valid identity proof
- Indoor slip
- Doctor’s prescription
- Patient’s photograph
- A copy of RSBY card or ration card for RSBY beneficiaries
- Discharge ticket
- A copy of medical test reports
Claim Procedure for Bhamashah Swasthya Bima Yojana:
BSBY is a cashless treatment scheme introduced by the Government of Rajasthan where the insurance company will bear all the medical expenses incurred by the beneficiaries. To avail the benefit of this scheme, the insured has to provide the policy card along with the personal ID proof while taking the admission in any network hospital. Apart from this, the insured will also need to provide the authorization from the insurer about his or her admission.
The hospital will start providing cashless treatment after the insurer has received the authorization. Once the treatment is done, the hospital will forward the medical reports, medical bills, physical certificate, and discharge summary to the insurance company for verification purpose. After the verification is done by the insurance company, the claim amount will be transferred to the network hospital.
What is Bhamashah Card?
Bhamashah card is a new scheme introduced by the Rajasthan government with the aim to make women the head of the family. The eldest woman of each family in the state will get this card. Once she received this card, the government will open a bank account in her name. The main motive behind this initiative is to create woman empowerment. Not only this but the government also provides financial grants directly by transferring them into their respective bank accounts. Bhamashah card should be linked to the beneficiary’s mobile number so that she can receive all the updates about the transactions that are happening through SMS.
How to Download Bhamashah Card?
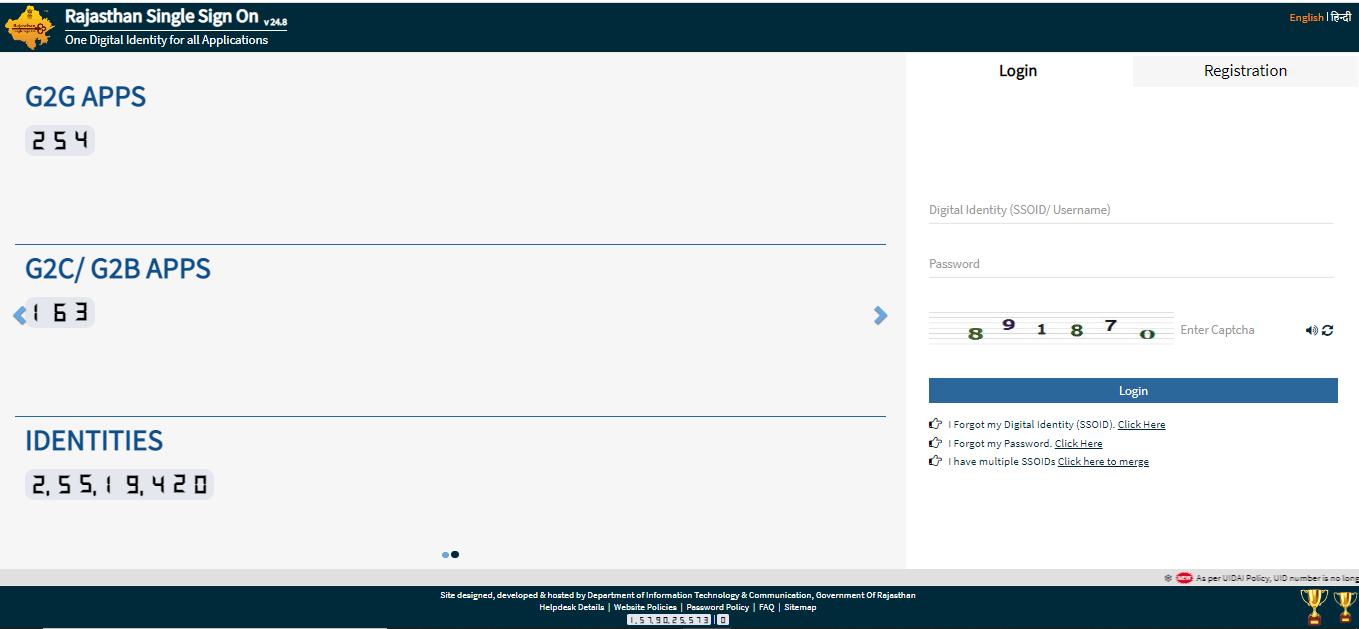
To download Bhamashah card, you need to register your name at the SSO Portal of Rajastha. Given below are the steps that you need to follow to download Bhamashah Card:
- Visit Government of Rajasthan
- Login to the portal using your SSO ID, password, and captcha code.
- Tap on ‘Citizen App’.
- Once you click on ‘Citizen App’, you will be able to view various options like Aadhar, Bhamashah, etc.
- Click on ‘Bhamashah’ option.
- Next, click on ‘E-Bhamashah Card’ option.
- You need to provide all the required information in the new page.
- Once done, you will be able to download your ‘Bhamashah Card’.
How to Update Bhamashah Card Bank Account?
The following are the steps to update Bhamashah Card bank account:
- Visit official website of Government of Rajasthan
- Login to your eMitra account using your login credentials.
- Tap on ‘Bank Detail’ option.
- Enter your ‘Bhamashah Receipt Number’.
- You will be redirected to a new page where you will be able to view your current bank account details.
- Now, you can make the required changes on your bank details.
What is the Activation Process of Bhamashah Card?
Follow the given steps to activate your Bhamashah Card:
- First, register your name under Bhamashah Yojana.
- Once, you have registered yourself, you need to select ‘Bhamashah Citizen Enrollment’.
- Now, enter your ‘Bhamashah Scheme Registration Number’.
- You will be redirected to the ‘Bhamashah Citizen Enrollment Form’.
- Enter all your required details, and click on ‘Submit’.
- Once you are done, with the above-mentioned steps, you will get a receipt number at your registered mobile number.
FAQs on Bhamashah Swasthya Bima Yojana
- What is the maximum insurance coverage provided under BSBY?
Under BSBY, the insured will receive up to Rs.30,000 for general illnesses and up to Rs.3 lakhs for critical illnesses.
- What is the transportation allowance for cardiac and polytrauma diseases?
The insurance company provides transportation allowance up to Rs.500 for cardiac and polytrauma diseases.
- I am a resident of Karnataka. Can I apply for Bhamashah Swasthya Bima Yojana?
No. Bhamashah Swasthya Bima Yojana is introduced only for the citizens of Rajasthan.
- What are the objectives of Bhamashah Swasthya Bima Yojana?
The main objective behind introducing Bhamashah Swasthya Bima Yojana is to make women financially independent.

Disclaimer
Credit Card:
Credit Score:
Personal Loan:
Home Loan:
Fixed Deposit:
Copyright © 2026 BankBazaar.com.
